BDI Score Guide: Next Steps After Your Depression Test Results
January 26, 2026 | By Beatrice Holloway
You have just finished the Beck Depression Inventory (BDI) and seen a number on your screen. But what does this number actually mean for your life? Seeing your score might feel overwhelming—particularly if it's higher than anticipated. Remember: This number is a starting point, not a label. You might be wondering if you should be worried or what the next logical step should be.
Understanding your depression screening results is the first step toward better emotional health. This guide is designed to help you move from curiosity to action. Whether your score was low or high, having a plan helps you feel more in control of your mental wellbeing.
At Bditest.org, we believe that self-awareness is the foundation of a richer life. If you haven't taken the assessment yet, you can take the confidential BDI assessment now to get your baseline score. If you already have your results, let’s dive into what those numbers mean and how you can use them to improve your daily life.
Understanding Your BDI Score: What the Numbers Mean
The BDI is one of the most trusted tools in the world for measuring the severity of depression. It looks at 21 different areas of your life, including your mood, sleep patterns, and how you feel about the future. However, it is important to remember that this is a screening tool, not a replacement for a conversation with a qualified professional.
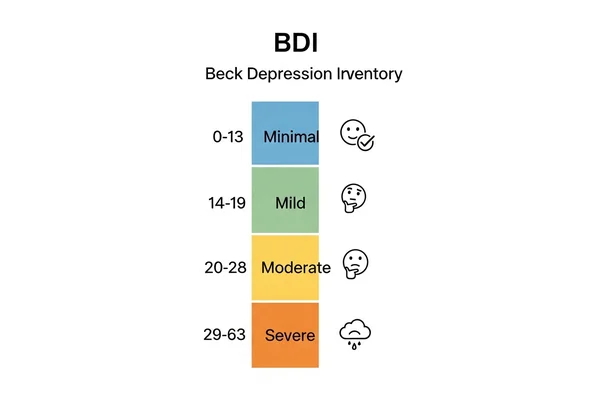
Breaking Down the BDI Score Ranges: Minimal, Mild, Moderate, and Severe Depression
The BDI uses a specific scale to categorize how you are feeling. These categories help you and health professionals understand the intensity of your symptoms. Here is the standard breakdown:
- 0–13: Minimal Depression. This range suggests you are experiencing normal ups and downs or very low levels of depressive symptoms.
- 14–19: Mild Depression. You may feel "off" or struggle with low energy. This sadness can start to interfere with your daily enjoyment.
- 20–28: Moderate Depression. Your feelings are valid, but they may be becoming increasingly difficult to manage. Symptoms likely affect your work, social life, or physical health.
- 29–63: Severe Depression. This indicates significant emotional distress. It is okay to seek support immediately to help navigate this intense period.
How Therapists Analyze BDI Test Patterns
Learn how clinicians use BDI patterns to gain deeper insight into your wellbeing. Doctors and therapists don’t just look at the total number; they look at the "patterns" in your answers. For example, a professional might notice if you scored very high on "sleep disturbance" but low on "guilt." This helps them understand if your depression is more physical or more cognitive in nature.
Clinicians also use these scores to track progress over time. Seeing your results shift from a 25 down to a 15 after therapy shows your treatment is working. It provides a clear way to measure progress between you and your provider. To get a head start, you can access your AI-powered report for a more detailed look at your specific responses.
External Factors Impacting Your BDI Score: Illness, Stress, and Honesty
Your score is a snapshot of how you have felt over the last week. Several things can temporarily change your results:
- Physical Illness: If you have the flu or a chronic pain flare-up, your scores for fatigue and sleep might be higher.
- Recent Life Events: Grief, a breakup, or losing a job can cause a temporary spike in symptoms.
- Hormonal Changes: Many people find their scores fluctuate during different parts of their biological cycles.
- Honesty: Your honesty when answering questions directly impacts the accuracy of your results.
Action Plan for Minimal Depression Scores (0-13)
If you scored in the 0–13 range, that is great news. It means your current emotional state is relatively stable. However, mental health is not a destination; it is a practice. Even with a low score, you can take steps to ensure you stay in a healthy range.
Daily Habits to Maintain Your Emotional Wellbeing
Preventative care is the best way to keep depression at bay. Focus on "The Big Three": sleep, movement, and connection. Try to get 7–8 hours of sleep and go for a 20-minute walk daily. Additionally, talk to at least one friend about something meaningful every day. These small habits create a "safety net" for your mood.
When to Re-take the BDI Test for Monitoring
We recommend that even those with minimal scores try our free tool every few months. Think of it like checking your blood pressure. If you go through a stressful period at work or school, doing a quick re-check can help you catch a downward trend before it becomes a serious problem.
Preventative Strategies to Keep Scores Low
Mindfulness and stress management are key. Practice saying "no" to over-commitment and set aside 10 minutes a day for deep breathing or meditation. By managing your stress levels now, you build emotional resilience for the future.
Responding to Mild Depression Scores (14-19)
A mild score is often a gentle "wake-up call." You might feel like you are functioning okay, but you aren't feeling like your usual self. This is the perfect time for early intervention, which can prevent symptoms from becoming more severe.
Early Intervention Techniques for Mild Symptoms
When depression is mild, it often responds well to "behavioral activation." This means doing things you usually enjoy, even if you don't feel like doing them right now. Start small—perhaps just listening to a favorite album or cooking a healthy meal. Action often leads to a shift in mood, rather than waiting for the mood to change first.
Lifestyle Changes That May Improve Your BDI Score
Check your "digital diet." Sometimes, spending too much time on social media or reading negative news can push a mild score higher. Try replacing 30 minutes of screen time with a hobby or a walk in nature. Additionally, reducing alcohol and caffeine can have a surprisingly large impact on mild depressive symptoms.
Warning Signs to Monitor as Your Score Increases
Keep an eye on your social withdrawal. If you find yourself canceling plans more often or if your work performance starts to slip, your depression may be moving into the moderate range. If you schedule a retest and see the numbers creeping up toward 20, it may be time to speak with a counselor.
Taking Action for Moderate Depression Scores (20-28)
If your score is between 20 and 28, you are likely feeling the weight of depression in your daily life. It is important to know that you don't have to "tough it out" alone. This level of depression is very common, and it is also very treatable.
When to Consider Professional Mental Health Support
If your score remains in the moderate range for more than two weeks, it is a strong signal to seek help. A therapist can provide you with tools like Cognitive Behavioral Therapy (CBT). This approach is specifically designed to challenge the negative thought patterns that the BDI measures.
How to Discuss Your BDI Results with a Healthcare Provider
You don't need to be an expert to talk to a doctor. Simply bring your score or a printout of your results to your appointment. You can say: "I took the Beck Depression Inventory online, and my score was 24. I’ve been feeling low for a while and would like to discuss my options." This gives your doctor a clear starting point for your care.
Self-Care Strategies for Managing Moderate Symptoms
While professional help is important, you can also support yourself at home. Focus on "radical self-compassion." Lower your expectations for yourself on bad days. If all you did was get out of bed and shower, that is a victory. Building a routine, however small, can provide a sense of stability when emotions feel chaotic.
Urgent Next Steps for Severe Depression Scores (29-63)
A score in the severe range means you are going through a very difficult time. It is vital to understand that severe depression is a health crisis, not a personal failure. There is hope, and there are people who want to help you through this.
Recognizing When Immediate Professional Help Is Necessary
If you are experiencing thoughts of self-harm, a complete inability to care for yourself, or a feeling of total hopelessness, please do not wait. Reach out to a professional immediately. A severe score on the BDI is an objective indicator that your brain is struggling, and you deserve medical support to get back on track.
Emergency Resources for Severe Depression
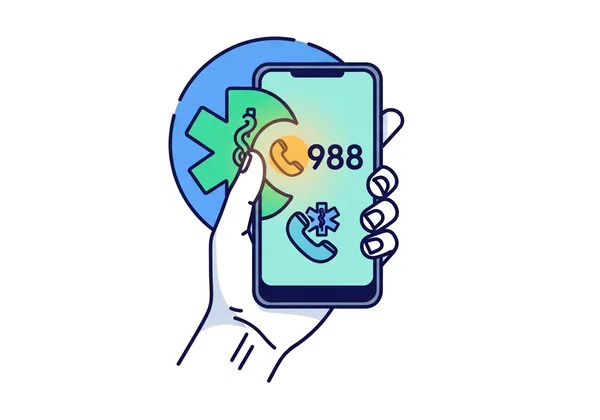
If you are in immediate distress, please utilize these free, confidential resources:
- National Suicide Prevention Lifeline (USA): Call or text 988.
- Crisis Text Line: Text "HOME" to 741741.
- International Resources: Search for "Crisis Hotlines" in your specific country for local support.
- Emergency Rooms: You can visit any hospital emergency room for mental health crises.
Support Options for Loved Ones of Those with Severe Scores
If you are reading this because someone you love took a test and received a high score, the best thing you can do is listen without judgment. Encourage them to see a doctor. Offer to help them make the appointment or drive them there. Your presence and validation can be a lifeline. If they are ready to talk about it, they can take the confidential BDI assessment to help identify the most pressing issues.
Key Takeaways: Using Your BDI Results to Improve Mental Health
Your BDI score offers a snapshot of where you are right now—but it's just the beginning of understanding your emotional health. Whether you scored a 5 or a 55, you now have the data you need to make informed decisions about your wellbeing. Remember, the BDI is a screening tool—it tells you where you are, but it doesn’t define who you are or where you are going.
Taking the time to check in with yourself is an act of courage. By using this guide, you have moved from simple curiosity to a concrete action plan. We encourage you to keep using our resources to stay informed. If you haven't yet received a detailed breakdown of your symptoms, you can access your AI-powered report to see a deeper analysis of your patterns.
Better mental health is a journey of small steps. You aren’t alone in this—support is always available. Take the next step today with confidence, knowing that clarity is within reach.
Frequently Asked Questions About BDI Scores
How often should I take the BDI test to monitor my progress?
For most people, taking the test once every two to four weeks is sufficient. If you are starting a new treatment or therapy, your provider might ask you to schedule a retest weekly to see how quickly you are responding to the changes.
Can my BDI score change over time, and what factors might affect this?
Yes, scores fluctuate frequently. Major life changes, physical health, sleep quality, and even the weather can impact how you answer the questions. The goal is to look for a "downward trend" in the numbers over several months, rather than worrying about a single day's spike.
What should I do if my BDI score suddenly increases?
If your score spikes unexpectedly, take a moment to consider recent stressors or changes in self-care habits. If the score stays high, it is a good idea to access your AI-powered report and discuss the results during a consultation with a therapist.
Is a BDI test enough to diagnose depression?
No. While the BDI is scientifically validated and highly accurate at measuring symptoms, a diagnosis requires a clinical interview with a licensed professional. They will look at your medical history and other factors that a digital test cannot capture.
How can I use my BDI results to track treatment progress?
Tracking scores in a journal helps visualize progress. Noticing a shift from 'Moderate' to 'Mild' can highlight your resilience during recovery. Many people find this incredibly encouraging during the slow process of healing. If you want to start tracking today, you can try our free tool to get your current baseline.