BDI Test & Sleep: Understanding Depression's Impact on Rest
November 11, 2025 | By Beatrice Holloway
Tossing and turning, watching the hours tick by, only to wake up feeling more exhausted than when you went to bed. This silent struggle with sleep is a heavy burden for many. It drains your energy, fogs your mind, and can make even simple tasks feel monumental. But what if these restless nights are more than just a passing phase? What if they are a crucial clue to understanding your overall mood? The connection between sleep and depression is profound, and the BDI test serves as an invaluable tool to shed light on this relationship. Have you ever wondered if your sleep problems are more than just a bad night?

For many, the quality of their sleep directly mirrors their mental well-being. Understanding this link is the first step toward finding clarity and taking control. On our platform, you can begin this journey of self-discovery with a free, confidential assessment. This guide will explore the deep-seated connection between depression and sleep, how the BDI test measures it, and what you can do to find rest. Taking this first step can provide the insight you need to move forward; you can start your self-assessment today.
Depression and Sleep: Unraveling the Vicious Cycle
The relationship between depression and sleep is not a one-way street; it's a vicious cycle. Poor sleep can worsen the symptoms of depression, and depression can make it nearly impossible to get a good night's rest. This frustrating loop can leave you feeling trapped and exhausted, making it difficult to find the energy to seek help or make positive changes.
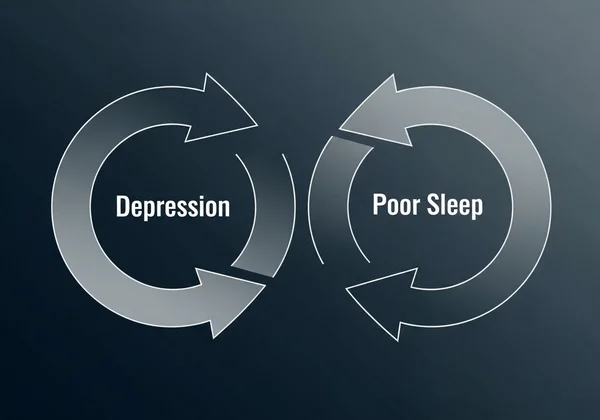
When your mood is low, your brain's delicate chemistry is often out of balance, which directly impacts the systems that regulate your sleep-wake cycle. This isn't just about feeling tired; it's a physiological response that often stems from an underlying emotional state. Breaking down this cycle begins with understanding its two main components: how depression physically affects your ability to sleep and the different ways these sleep disturbances can manifest.
Why Sleep Suffers During Depression: The Brain's Role
At the heart of both mood and sleep regulation are neurotransmitters—the brain's chemical messengers. Key players like serotonin, norepinephrine, and dopamine are crucial for maintaining a stable mood, but they also help manage your sleep patterns. When you're experiencing depression, the levels and activity of these neurotransmitters can become dysregulated, sending mixed signals throughout your brain.
Furthermore, depression is often linked to an overactive stress response system, leading to elevated levels of the stress hormone cortisol. High cortisol levels, especially at night, can cause a state of hyper-arousal, making it incredibly difficult to relax and fall asleep. Your body remains on high alert, even when you're desperate for rest, perpetuating a cycle of exhaustion and low mood.
Insomnia vs. Hypersomnia: Two Sides of Depressive Sleep Issues
When sleep problems arise with depression, insomnia—the persistent difficulty falling or staying asleep, or waking too early—is often the first thing people think of. This is one of the most common signs of depression sleep issues. The racing thoughts, feelings of anxiety, or a sense of profound sadness can make the quiet of the night feel overwhelming, turning your bed into a place of stress rather than sanctuary.
However, depression can also manifest as its opposite: hypersomnia, or sleeping too much. This isn't restful, restorative sleep. Instead, it's often a form of escape, where sleep becomes a retreat from painful emotions and a world that feels overwhelming. Despite logging extra hours in bed, individuals with hypersomnia often wake up feeling unrefreshed, groggy, and even more fatigued, further feeding into the cycle of depression. To explore your symptoms further, a structured tool can be incredibly helpful.
How the BDI Test Assesses Sleep Disturbance
So, how do we move from feeling tired to understanding if it’s a symptom of something more? This is where a scientifically validated tool like the Beck Depression Inventory (BDI) becomes essential. The BDI sleep disturbance questions are designed not just to ask if you're tired, but to quantify the changes in your sleep and energy levels in a way that provides meaningful insight.
The BDI test is a comprehensive self-assessment that looks at 21 common symptoms of depression. It provides a holistic view of your emotional and physical state, and a few key questions are specifically designed to evaluate how your mood is impacting your rest and daily energy. It helps you connect the dots between how you feel and how you function.
BDI Question 16: Exploring Your Sleep Patterns
One of the most direct measures of sleep on the BDI is Question 16. This item asks you to compare your current sleep patterns to your usual ones. The answer choices are carefully crafted to capture the full spectrum of sleep disturbances seen in depression.
The options range from sleeping the same as usual to sleeping slightly more or less, and significantly more or less. This allows the test to identify both insomnia (sleeping less) and hypersomnia (sleeping more). By scoring your response, the BDI provides a concrete measure of how much your sleep has deviated from your personal baseline, offering a vital clue into your overall well-being.
BDI Question 18: Energy and Fatigue Explained
Poor sleep inevitably leads to fatigue, another core symptom of depression. BDI Question 18 directly addresses this by assessing your energy levels and how easily you get tired. It recognizes that the impact of poor sleep is just as important as the sleep disturbance itself. Waking up exhausted day after day takes a toll on your motivation, concentration, and ability to engage with life.
This question helps quantify that experience, from feeling no more tired than usual to feeling too tired to do most of the things you used to do. It connects the dots between a night of poor rest and a day of low energy, painting a clearer picture of depression's effect on your daily life. If you want to see the test questions and how they relate to your experience, the full assessment is available online.
Interpreting Your BDI Sleep-Related Scores
Scoring high on Questions 16 and 18 can be a strong indicator that your mood is significantly affecting your sleep and energy. However, it's crucial to remember that the BDI's strength lies in its overall score. The test is designed to identify a pattern or cluster of symptoms. A high score on sleep-related items, combined with scores on items related to sadness, loss of interest, or self-criticism, provides a much more comprehensive and reliable picture.
The BDI test is a screening tool, not a diagnostic one. Its purpose is to give you valuable, personalized information to better understand your own experience and to serve as a starting point for a conversation with a healthcare professional. To see how your symptoms form a pattern, you can get your BDI score instantly and confidentially.
Beyond the BDI: Practical Steps for Better Sleep & Mood
Gaining insight from a tool like the BDI test is a powerful first step. It empowers you with knowledge about what you're experiencing. The next step is to use that knowledge to make positive changes. While these practical tips are not a substitute for professional medical advice, they can help support better sleep and, in turn, a better mood.
Think of these strategies as building a healthier foundation for your mind and body. Improving your sleep hygiene can help calm your nervous system and create a more conducive environment for rest, which can be especially beneficial when you're managing symptoms of depression.
Essential Sleep Hygiene Tips for Depression Management
Sleep hygiene refers to the habits and practices that are conducive to sleeping well on a regular basis. When you’re struggling with your mood, consistency is key.

- Stick to a Schedule: Go to bed and wake up at the same time every day, even on weekends. This helps regulate your body's internal clock.
- Create a Restful Environment: Make sure your bedroom is dark, quiet, cool, and comfortable. Use blackout curtains, earplugs, or a white noise machine if needed.
- Develop a Relaxing Bedtime Routine: Spend the hour before bed doing something calming, like reading a book, taking a warm bath, or listening to gentle music. Avoid screens, as the blue light can interfere with sleep.
- Watch What You Eat and Drink: Avoid large meals, caffeine, and alcohol close to bedtime. They can disrupt your sleep cycle later in the night.
When to Seek Professional Help for Sleep and Depression
While self-assessment and lifestyle adjustments are valuable, it's important to recognize their limits. If your sleep problems and low mood persist, significantly impact your ability to work or maintain relationships, or if you feel overwhelmed, it is essential to seek professional help. Your BDI test results can be an excellent way to start the conversation with a doctor, therapist, or counselor.
A professional can provide an accurate diagnosis and create a treatment plan tailored to your specific needs, which may include therapy, medication, or other interventions. Remember, reaching out for help is a sign of strength and the most effective step you can take toward feeling better.
Your Journey to Better Sleep and Understanding Your Mood
The link between how you sleep and how you feel is undeniable. Restless nights and exhausted days are often more than just physical symptoms—they are important messages from your mind. By paying attention to them, you can begin a journey of self-discovery and healing.
The BDI test offers a clear, confidential, and scientifically validated way to explore this connection. It translates your feelings into tangible insights, empowering you with the knowledge to take the next step. You don't have to navigate this journey alone or in the dark. Clarity and a path forward can begin right here.
Ready to understand your mood and its impact on your sleep? Take the free BDI test today to receive your immediate results and begin your path to a brighter, more rested tomorrow.
Frequently Asked Questions About BDI, Sleep, and Depression
What is the BDI test for?
The BDI test is a widely used self-assessment tool designed to measure the severity of depressive symptoms. It is a screening instrument that helps individuals gain insight into their emotional well-being and can be used to track symptoms over time. It's not a diagnostic tool, but it offers a valuable and confidential starting point for self-understanding and for conversations with a healthcare professional.
Is the BDI test scientifically valid?
Yes, the Beck Depression Inventory is one of the most respected and scientifically validated instruments for measuring depression. Developed by Dr. Aaron T. Beck, it has been used in thousands of research studies and clinical settings for decades, demonstrating its reliability and accuracy in assessing depressive symptomatology.
Can poor sleep be a direct sign of depression?
Absolutely. Changes in sleep patterns, including both insomnia (difficulty sleeping) and hypersomnia (excessive sleeping), are considered hallmark symptoms of depression. While other factors can cause poor sleep, a persistent disruption combined with a low mood is a strong indicator that should be explored further.
What is a "normal" BDI score regarding sleep issues?
There isn't a specific "normal" score for the sleep questions alone. The BDI works by looking at the total score from all 21 questions. Generally, a lower overall score (e.g., 0-13) indicates minimal or no depressive symptoms, which would typically include normal sleep patterns. The key is to see how sleep issues contribute to your overall score.
How can I improve my sleep when I'm feeling low?
Improving sleep while managing a low mood often involves a two-pronged approach. First, practice good sleep hygiene, such as maintaining a consistent schedule and creating a relaxing bedtime routine. Second, address the underlying mood issues. Taking a BDI test to understand your symptoms can be a great first step before speaking with a professional who can recommend targeted treatments like therapy or medication. You can learn more about BDI on our website.