Clinical Use of BDI: Guide for Professionals & Students
October 30, 2025 | By Beatrice Holloway
To effectively assess mental health, you need reliable, scientifically validated tools. For professionals, students, and researchers in mental health, the Beck Depression Inventory (BDI) is a cornerstone instrument. This comprehensive guide will show you how to leverage the clinical use of BDI in your practice, from initial screening to monitoring treatment progress. If you've ever asked, What is the BDI test for?, you'll find a deep understanding of its application, interpretation, and ethical use here, empowering you to use this tool effectively. For a reliable and accessible version, feel free to explore our platform.

The BDI's Foundational Role in Clinical Practice
The Beck Depression Inventory isn't just another questionnaire. It's a meticulously designed tool that has transformed how we understand and measure depressive symptoms. Its widespread use is a testament to its robust psychometric properties and clinical utility. For decades, it has bridged a patient's subjective experience with objective data to inform your clinical decisions.
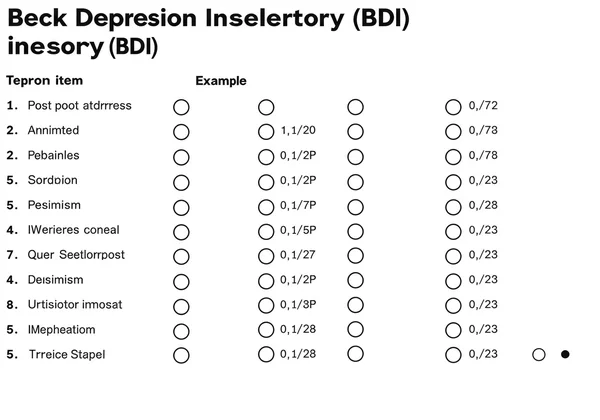
What is the Beck Depression Inventory? Understanding its Design
Dr. Aaron T. Beck developed the BDI as a 21-item, self-report inventory to measure the severity of depression. Each item corresponds to a specific symptom or attitude, such as sadness, pessimism, guilt, and fatigue. Your clients rate each item on a 4-point scale, reflecting their experiences over the past week. The clear design and focus on concrete symptoms make the BDI test questions easy for clients to understand and for you to analyze.
BDI's Scientific Validity: A Cornerstone of Reliable Assessment
The BDI's prominence stems from its strong scientific validity and reliability. Countless studies prove its effectiveness in distinguishing between depressed and non-depressed individuals and its correlation with other depression measures. This empirical backing ensures that when you use the BDI, you are using a tool that provides meaningful and consistent results. This validation is a trustworthy foundation for both clinical assessment and academic inquiry and is critical when considering a BDI online tool.
BDI vs. BDI-II: Key Differences and Evolution
In your practice, you may encounter two versions: the original BDI and the revised BDI-II. Updated in 1996, the BDI-II aligns more closely with the DSM-IV diagnostic criteria for depressive disorders. Key changes include modified items assessing symptoms like agitation and worthlessness and extending the timeframe to the past two weeks. While both versions are valid, the BDI-II test is now more commonly used in clinical and research settings because of its updated criteria.
Practical Applications: BDI for Therapists & Clinicians
In a therapeutic setting, the BDI is a versatile tool that supports every stage of your clinical workflow. It gives you a structured way to gather essential information, foster client collaboration, and make data-driven decisions about their care. Its efficiency helps you gain valuable insights quickly.
Utilizing BDI for Initial Screening and Symptom Identification
A primary use of the BDI is for initial screening. When a new client presents with vague complaints of feeling down, the BDI can quickly help you identify the presence and severity of depressive symptoms. It provides a comprehensive snapshot of their condition, highlighting specific concerns—like suicidal ideation or anhedonia—that require immediate attention. This initial screening is a crucial first step, made simple with an online BDI test.
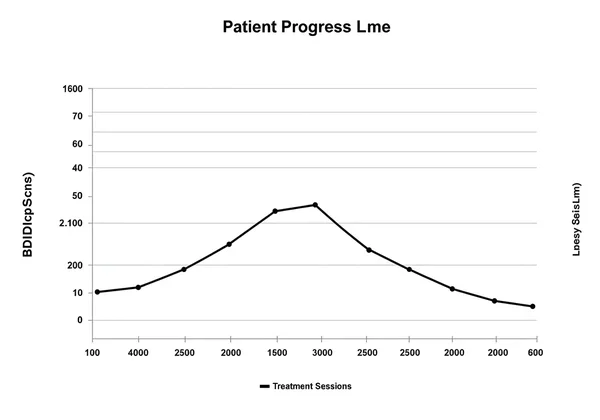
Monitoring Patient Progress and Treatment Effectiveness
The BDI is invaluable for tracking your client's therapeutic journey. By administering it at regular intervals—such as intake, mid-treatment, and termination—you can objectively measure changes in symptom severity. This data provides concrete evidence of treatment effectiveness, helping you decide if the current approach is working or needs adjustment. It also empowers clients by letting them see their own progress.
Guiding Clinical Interviews and Tailoring Treatment Plans
BDI results are more than just a number; they're a roadmap for your sessions. A high score on an item like "self-criticism" can guide your line of questioning during a clinical interview, allowing for a deeper exploration of your client's core beliefs and behaviors. These specific insights help you tailor treatment plans more effectively, focusing interventions on the most distressing symptoms.
Interpreting BDI Scores: A Professional's Guide
To interpret BDI scores accurately, you need to go beyond the standard cutoffs. True understanding involves seeing what the scores mean in the context of an individual's life, clinical presentation, and cultural background. The total score is just the starting point for a much deeper clinical investigation.
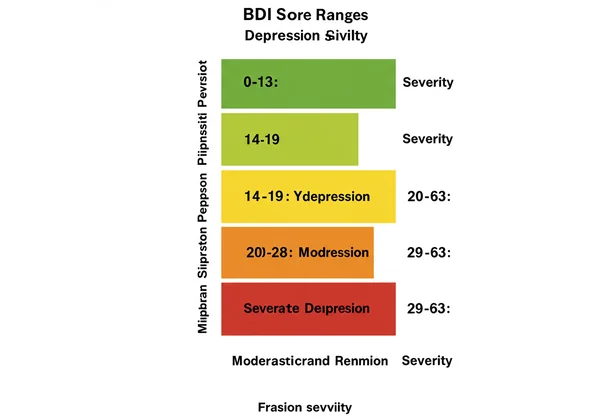
How to Calculate BDI Scoring and Understand Severity Levels
BDI scoring is straightforward. Each of the 21 items is scored from 0 to 3, with the total score being the sum of all ratings (0 to 63). These scores are categorized into severity levels, providing a clear assessment framework.
- 0-13: Minimal depression
- 14-19: Mild depression
- 20-28: Moderate depression
- 29-63: Severe depression
These ranges for BDI mild moderate severe levels help clinicians quickly classify symptom severity and determine an appropriate level of care.
Beyond the Number: Qualitative Interpretation of BDI Score Meaning
While the total score is important, the real clinical richness comes from analyzing the response patterns. Which specific symptoms are most pronounced? Are they primarily cognitive (like pessimism) or somatic (like fatigue)? Understanding this qualitative data gives you a more holistic view of the client's experience. This deeper BDI score meaning helps you formulate a more precise, personalized therapeutic strategy, which can begin with a simple self-assessment.
What is a "Normal" BDI Score? Contextualizing Results
You might often hear, "What is a normal BDI score?" While scores in the minimal range (0-13) are typical for non-clinical populations, it's crucial to avoid labeling scores as "normal" or "abnormal." You must always interpret a score within the client's individual context, considering factors like recent stressors, medical conditions, and cultural background. The BDI identifies the level of distress, not a deviation from a rigid norm.
Beck Depression Inventory for Research and Ethical Considerations
Beyond clinical practice, the BDI is a vital research tool that helps advance our understanding of depression. However, using it in any professional context—clinical or academic—must be guided by strict ethical principles to protect individual well-being and privacy.
Methodological Applications: Using BDI for Academic Inquiry
In research, the BDI is used to screen participants for studies, measure outcomes in clinical trials, and explore the correlates of depression. Its reliability and validity make it a gold standard for quantifying depressive symptoms in scientific investigations. Its availability in multiple languages on online BDI test platforms further enhances its utility for cross-cultural research.
Upholding Ethics: Confidentiality and Informed Consent in BDI Use
When you administer the BDI, ethical practice is paramount. You must obtain informed consent, explaining the test's purpose, how results will be used, and who can access them. Confidentiality is non-negotiable. Using a secure BDI platform helps ensure you handle client data with the required privacy and security.
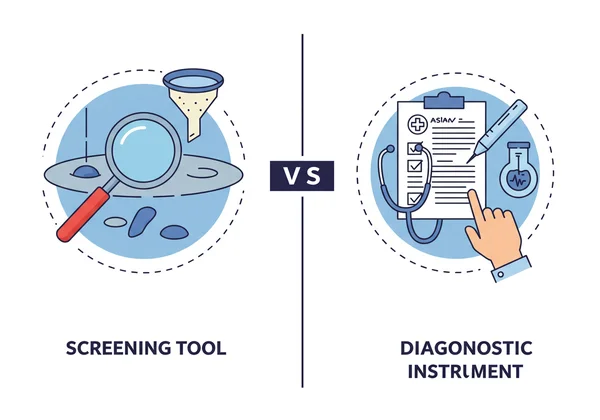
BDI as a Screening Tool: Not a Standalone Diagnostic Instrument
It cannot be overstated: the BDI is a screening tool, not a diagnostic instrument. While it measures the severity of depressive symptoms, it does not provide a clinical diagnosis of Major Depressive Disorder. A diagnosis can only be made by a qualified healthcare professional after a comprehensive evaluation. You must communicate this distinction clearly to clients to manage expectations and encourage them to seek a full assessment.
Empowering Your Practice with the BDI: Informed Assessment & Ethical Care
The Beck Depression Inventory is an indispensable asset for you, whether you are a professional, student, or researcher in mental health. From initial screening and treatment planning to monitoring progress and conducting research, its applications are broad and deep. By understanding how to administer, score, and interpret the BDI within an ethical framework, you can enhance your quality of care and contribute to better mental health outcomes. To integrate this powerful tool into your practice, consider using a reliable free BDI test.
Frequently Asked Questions on BDI Clinical Use
What is the primary clinical use of the BDI in patient care?
Its primary clinical use is to quickly and reliably screen for the presence and severity of depressive symptoms. It helps you identify at-risk individuals, monitor their progress during treatment, and make informed decisions about their care plan.
How does the BDI's scientific validity support its use in professional settings?
Its extensive validation confirms it accurately measures depressive symptoms. This scientific backing gives you confidence that the results are reliable and meaningful, making it a trustworthy tool for both clinical assessment and academic studies.
What are the key steps to interpreting a client's BDI scores accurately?
Accurate interpretation involves three key steps: calculate the total score for severity, analyze response patterns to identify specific symptoms, and contextualize the results within the client's personal history and current situation. You can support this process with a standardized assessment tool online.
Is there a significant difference between the BDI and BDI-II for clinical application?
Yes. The BDI-II is updated to better align with modern diagnostic criteria (DSM-IV), making it the preferred version for most clinical applications. It includes revised items for a more comprehensive assessment of depressive symptoms.
What ethical considerations are paramount when administering the BDI?
The most critical ethical considerations are obtaining informed consent, ensuring client confidentiality, and clearly communicating that the BDI is a screening tool, not a diagnosis. You must always emphasize the importance of a full evaluation by a qualified expert.